Male Diagnosis
Infertility is a widespread problem. It is usually considered as a female problem, but in fact, in about 25% of an infertile couple the problem lies solely in male partners and another 15-25% is the male contribution.

Male infertility can be due to any of the following reasons:
The most common cause of infertility. Either there is no production or very low sperm production or sperm do not have the ability to fertilize the egg. This could be due to genetic problems, varicocele, high temperature in the groin area, undefended testes during birth, etc
Though there is normal sperm production, but due to blockage in the passage from testis to penis, can cause lack of sperm in the ejaculated sample. This could be due to vasectomy, or absence of vas deferens or any recent infections
Erection or ejaculatory problem, retrograde ejaculation, spinal cord injury etc. can be one of the
factors for infertility.
FSH, LH, Testosterone are important hormones for sperm production. Sub-optimal levels of these hormones can affect sperm quantity and quality.
Antibodies are developed, when the immune system reacts against man’s own sperm, considering it as a foreign cell. These antibodies cause clumping of sperm cells and restrict its motility (movement).
High levels of stress, performance pressure, unhealthy lifestyle, serious illnesses, drugs, or chemotherapy could all contribute to lowering your chances of conceiving the natural way.
Complete diagnostic work is required to identify and treat the condition. Diagnostic workup involves a detailed medical history, physical examination, basic and specialized tests.
A. Basic Test:
Semen Analysis:
It is a single most useful and gold standard test to evaluate male infertility. It provides insight into the sperm production (Count) and sperm quality (Motility and morphology). It helps to assess the maturity of sperm and also about its interaction with the seminal fluid.
Before semen analysis, it is recommended to maintain abstinence of 2-7 days. The sample should be produced in the clinic. Masturbation is the best way of sample collection as the entire sample is collected, especially the sperm rich first portion.
Semen Analysis involves:
- Macroscopic analysis- to assess liquefaction, volume ,pH, viscosity
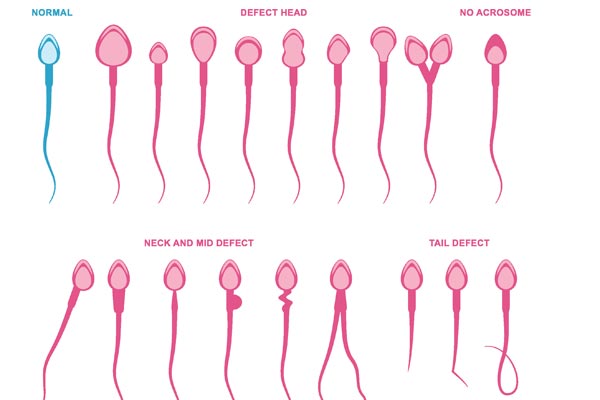
- The microscopic analysis includes sperm number (Count), movement of sperm (Motility), the shape of sperm (Morphology), the viability of sperm (Vitality), presence of round cells, antibodies
Semen Culture:
Semen culture is a laboratory test, which helps in identifying the presence of micro-organism in the semen sample. The test report is available in 3-5days.
Test Report:
- No Growth :
- Indicates that the semen sample has no micro-organism
- Presence of Growth :
- indicates presence of micro-organism. In the test report the name of the micro-organism and its effective antibiotics will be mentioned.
B: Specialized Test:
Hormonal Tests:
- Blood test to check the hormone level namely FSH, LH, and Testosterone
Sperm Chromatin Dispersion test:
- to assess sperm DNA fragmentation
Genetic Tests:
- Karyotyping, Y-Chromosome micro-deletion
The World Health Organization (WHO 2010) reference level (modified):
| Semen parameter | Meaning | Reference Range |
|---|---|---|
| Volume | The total amount of fluid ejaculated | ≥1.5 mL |
| Total sperm number | The number of sperm in the entire ejaculate | ≥39 million |
| Sperm count | The number of sperm per ml of semen | ≥15 million per ml |
| Total motility (Progressive + Non- Progressive motility | The ability of sperm to move actively and all other patterns of movement e.g. Moving in small circles, flagellar beat | ≥40% |
| Progressive Motility | The ability of sperm to move actively | ≥32% |
| Sperm morphology | Shape of the sperm | ≥4% |
| Semen pH | Measured to test if the ejaculate is acidic or alkaline. Semen should be slightly alkaline. | ≥7.2 |
